Capitolwire: Action on Mental Health Funding Uncertain With House Control Up for Grabs
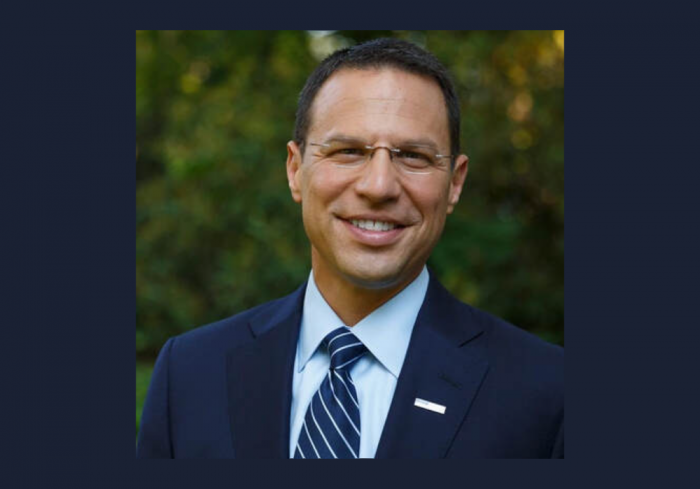
RCPA President and CEO Richard Edley Named to Gov.-Elect Shapiro’s Human Services Advisory Committee
Governor-Elect Josh Shapiro and Lieutenant Governor-Elect Austin Davis have announced the members of seven Transition Advisory Committees, “which will advise the incoming Administration and prepare to advance Governor-Elect Shapiro’s top priorities.” Richard Edley, President and CEO of RCPA, has been named to the Health and Human Services Advisory Committee. Several RCPA members, associates, and partners have also been named across the committees. Per the announcement:
“Governor-Elect Josh Shapiro and Lieutenant Governor-Elect Austin Davis have assembled a diverse and experienced team of Pennsylvania leaders and policy experts to advise their transition on a wide array of different policy areas to help move the Commonwealth forward. From public safety to economic development, the Transition Advisory Committees will play a key role in ensuring the Administration is ready to tackle these priorities.”
Read the full press release here.
Capitolwire: Date Set for Special Election for Senate Seat, While House Leaders Squabble Over Date of House Special Election
Capitolwire: Shapiro Names Fritz as His Chief of Staff
State Senator John Gordner Resigns
Shapiro Transition Team Pulls in Experience From Democratic and Republican Administrations
Capitolwire: House GOP Keeps Cutler as Leader
Capitolwire: Democrats Stand to Gain Majority in House, But They May Not Be Able to Immediately Take Control of the Chamber
PA Gov.-Elect Josh Shapiro, Lieutenant Gov.-Elect Austin Davis Make Transition Announcements
HARRISBURG, Pa. — Pennsylvania Gov.-elect Josh Shapiro and Lieutenant Gov.-elect Austin Davis held a news conference Wednesday to announce the first steps in the transition to their incoming administration.
Outgoing Gov. Tom Wolf joined Shapiro and Davis for the announcement at the state Capitol in Harrisburg.
Shapiro and Davis will be sworn in on Jan. 17. The transition team will include executive director Akbar Hossain, who was the policy director on Shapiro’s gubernatorial campaign, and communications director Manuel Bonder, who was Shapiro’s campaign press secretary. Directing the inauguration will be Amanda Warren, who served as finance director on the campaign.
Shapiro also announced a transition website, shapirodavis.org, encouraging Pennsylvanians to learn more about the inauguration and to apply for roles in the new administration.
Shapiro is currently the state attorney general, and his term ends in January 2025. The governor will nominate someone to fill out the term, and that person will need Senate approval. The first deputy will take over the duties of attorney general until the position is filled.
Currently a state representative for the 35th District, Davis was reelected to that office in last week’s election while he also ran for lieutenant governor. A special election will be held to replace Davis in the state House.