Welcome! Login in to your account
Register for an account
A password will be e-mailed to you.
Recover your password
Home In the News
B-PEP Calls On Gov. Wolf to Consider Blacks for Bench Openings
RCPA Member Vista Autism Services Announces New CEO
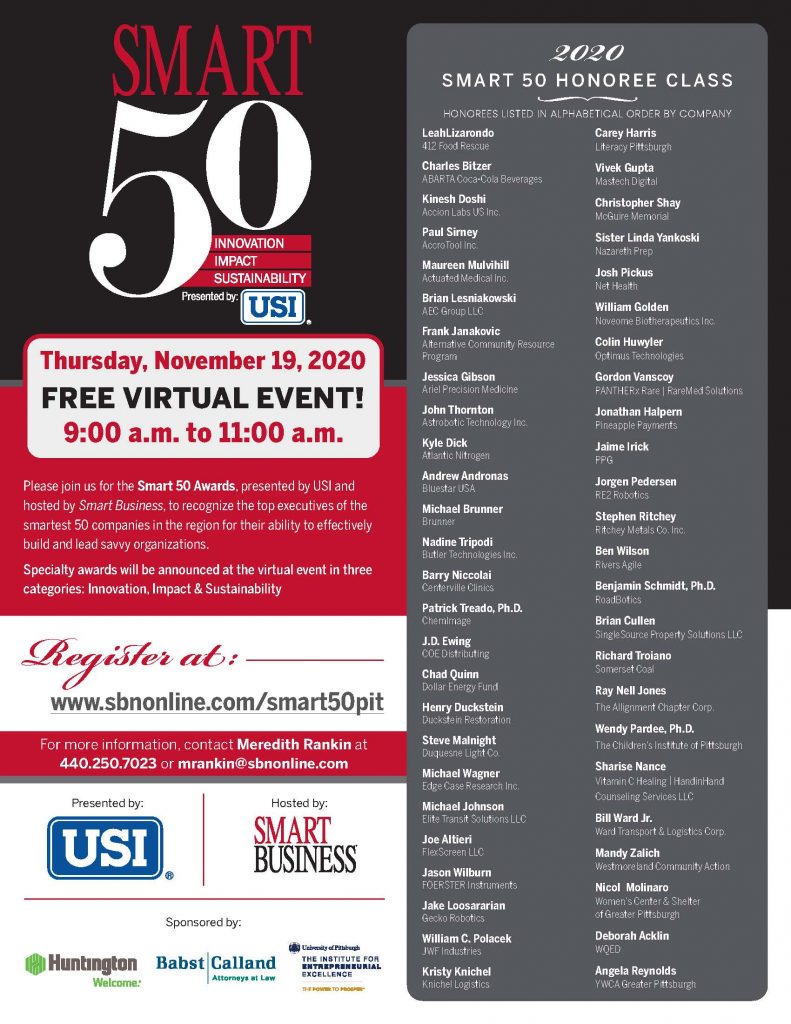
Member News from ACRP and Frank Janakovic
Who Will Get a COVID-19 Vaccine First? PA Outlines Plans to Distribute Coronavirus Shot.
Amid COVID-19 Cases and Restrictions, Nursing Homes See Rise in Deaths by Neglect
COVID Vaccine Could Be Ready for Rollout in Pennsylvania Next Month, Health Secretary Says

Food Safety, COVID-19 Precautions For Thanksgiving and Travel Mitigation Effort
Spit Test May Diagnose Concussions in Athletes
Congratulations to RCPA Member Access Services, Inc. and their new CEO, Sue Steege!
© 2021 - Rehabilitation & Community Providers Association