Advance Rates for NatCon26 End March 12



RCPA has been a long-time partner of the Center for Health Care Strategies (CHCS), a policy design and implementation organization devoted to improving outcomes for people enrolled in Medicaid. Our collaborative efforts across the arena of Medicaid and the pending impacts of HR 1 remain a critical connection point to ensure access in Pennsylvania.
On behalf of CHCS, RCPA would like to share this update on resources related to the Rural Health Transformation Project. Per the update:
The federal Rural Health Transformation Program (RHTP), authorized under the 2025 budget reconciliation act (P.L. 119-21), will distribute $50 billion to all 50 states from 2026 to 2030 — serving as a partial offset to Medicaid cuts. In designing and launching RHTP plans, state agencies must meet ambitious federal expectations and timelines. Experiences from other large-scale statewide efforts — such as the American Rescue Plan Act, Opioid Settlement Funds, multisector plans for aging (MPA), and the Centers for Medicare & Medicaid Services’ (CMS) State Innovation Models (SIM) demonstration — can help inform state planning.
This brief provides practical recommendations to help states establish the administrative infrastructure needed to implement their RHTP plans. Drawing on insights from state officials involved with similar transformation efforts, as well as the Center for Health Care Strategies’ (CHCS) experience supporting this work, the brief highlights best practices and common pitfalls across four core domains:
While not exhaustive, this brief outlines practical lessons that state staff can use to guide RHTP activities during the critical first six to nine months of program design and implementation, helping states build a strong foundation for long-term success.
Additionally, CHCS published a series of tip sheets to aid stakeholders in exploring strategies and initiatives within the project. The tip sheets offer resources for strengthening rural health, including workforce and access issues.
If members have any questions regarding this update or the Rural Health Transformation Plan, please contact RCPA COO Jim Sharp.
RCPA continues to seek proposals for the 2026 Annual Conference Power in Purpose: Promoting Possibilities, which will be held September 29 – October 2 at the Hershey Lodge for a statewide audience. RCPA’s Conference Committee is looking for workshop proposals in every area for possible inclusion, particularly those that assist providers in developing and maintaining high-quality, stable, and effective treatments, services, and agencies in an industry where change is constant. The committee looks for presentations that:
 Highlight new policy, research, and treatment initiatives, such as the use of artificial intelligence and technology in service provision;
Highlight new policy, research, and treatment initiatives, such as the use of artificial intelligence and technology in service provision;The committee welcomes any proposal that addresses these and other topics essential to brain injury, medical rehabilitation, mental health, substance use disorder treatment, children’s health, aging, physical disabilities, autism, and/or intellectual/developmental disabilities. Members are encouraged to consider submitting, and we highly encourage you to forward this opportunity to those who are exceptionally good speakers and have state-of-the-art information to share.
The Call for Proposals (featuring a complete listing of focus tracks) and accompanying Guidelines for Developing Educational Objectives detail requirements for submissions. The deadline for submissions is COB Monday, March 23, 2026. Proposals must be submitted electronically with the form provided; confirmation of receipt will be sent. Proposals submitted after the deadline may not be considered.
 If the proposal is accepted, individuals must be prepared to present on any day of the conference. Workshops are 90 minutes in length. If the topic requires an in-depth presentation, a double session can be scheduled for a total of 180 minutes. At the time of acceptance, presenters will be asked to confirm the ability to submit workshop slides and handouts electronically two weeks prior to the conference. Individuals unable to meet this expectation may not have their materials available to participants during the conference.
If the proposal is accepted, individuals must be prepared to present on any day of the conference. Workshops are 90 minutes in length. If the topic requires an in-depth presentation, a double session can be scheduled for a total of 180 minutes. At the time of acceptance, presenters will be asked to confirm the ability to submit workshop slides and handouts electronically two weeks prior to the conference. Individuals unable to meet this expectation may not have their materials available to participants during the conference.
Individuals are welcome to submit more than one proposal; however, we ask that you submit no more than three total. Notification of inclusion for the conference will be made via email by Monday, May 11, 2026. Questions may be directed to Carol Ferenz, Conference Coordinator.
With support from the Preschool Development Grant, the Office of Child Development and Early Learning (OCDEL) is supporting a training initiative to help build a cross-disciplinary workforce across Pennsylvania that understands very young children’s mental health and development and can provide better, more informed support to families and caregivers.
You, or a Children First PA representative(s) of your choosing, are invited to participate in an upcoming DC:0–5™: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood Overview webinar. This 90-minute session is designed for policy leaders, advocates, and human services administrators who play a pivotal role in shaping systems that support the mental health and well-being of our youngest children.
About the Training:
The DC:0–5™ framework provides a developmentally sensitive approach to understanding and classifying mental health and developmental disorders in children from birth through age five. The overview will:
Why Your Participation Matters:
Your leadership and expertise are essential in ensuring that policies and programs reflect the latest understanding of infant/early childhood mental health. By engaging in this training, you will be better equipped to:
DATE: February 18, 2026, from 2:00 pm – 3:30 pm EST
Participants will need to create a free eLearn account with ZERO TO THREE if they do not already have one to complete their registration.
Priority registration is available through February 11, 2026, before the training announcement is made public the following day. Space is limited to 100 attendees.
We look forward to your participation in this important conversation and to working together to advance the well-being of young children and their families. If you cannot attend this session, there will be additional opportunities in 2027, as this initiative also includes a Training of Trainers strategy.
If you have any additional questions, please contact RCPA COO Jim Sharp.
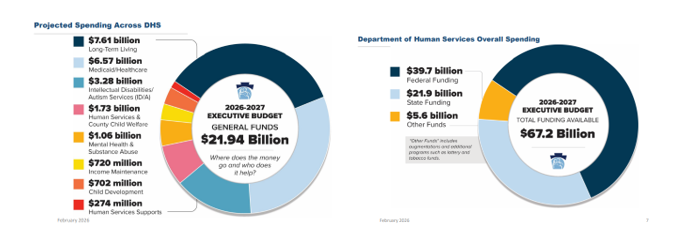
On Friday, February 6, Department of Human Services (DHS) Secretary Val Arkoosh presented an overview of Governor Shapiro’s proposed Fiscal Year (FY) 2026/27 budget and detailed the projected spending across DHS, which totals $21.94 billion in state funding. The Secretary highlighted that all three Medicaid managed care programs, as well as waiver programs for people with intellectual disabilities and autism, are receiving increases, largely driven by patient needs and costs associated with delivering care. The proposed FY 2026/27 budget includes $39.7 billion in federal funding as well as $5.6 billion from augmentations and additional programs, such as lottery and tobacco funds, making the total DHS funding $67.2 billion.
The Secretary expressed how the proposed budget reflects the direct impacts of HR 1, with significant federal funding at risk. The distribution for the 2026/27 budget is based upon the current structure of Medicaid and other federally funded programs, but the Secretary noted that beginning in 2028, changes in Medicaid financing rules will remove $20 billion from Pennsylvania’s Medicaid program over the following decade.
Budget Highlights and Investments
Due to technical difficulties, DHS was unable to record the webinar, but the presentation slides and transcript can both be viewed.
Please contact your RCPA Policy Director with any questions or concerns.

The Office of Mental Health and Substance Abuse Services (OMHSAS) has announced an upcoming learning opportunity from the Youth and Family Training Institute (YFTI) that may be valuable to workforce, providers, educators, and anyone supporting children, youth, and families.
On February 18, 2026, from 12:00 pm – 1:30 pm, YFTI will host Foundations of Family Driven Teaming Approaches, a free webinar designed to strengthen understanding of how to partner with families in meaningful, collaborative, and effective ways.
This session will introduce participants to:
Family Driven Teaming places the family’s voice, culture, and priorities at the center of planning and decision making. This approach strengthens engagement, improves outcomes, and helps families build sustainable skills and relationships beyond formal services.
Register for Foundations of Family Driven Teaming Approaches
Questions and comments can be sent electronically.
The Office of Mental Health and Substance Abuse Services (OMHSAS) has announced that Psychiatric Rehabilitation Services (PRS) has been added to the Medical Assistance Program Fee Schedule, effective January 1, 2026.
On January 30, 2026, the Centers for Medicare & Medicaid Services approved the addition of PRS as a rehabilitative service to the Medicaid State Plan, leading to the issuance of OMHSAS-26-01, “Payment for Psychiatric Rehabilitation Services.” Prior to the inclusion in the Medicaid State Plan, PRS was available only to MA beneficiaries enrolled in Behavioral Health HealthChoices as an in lieu of service. PRS is now available as a state plan service to MA beneficiaries in the Fee-for-Service and Behavioral Health HealthChoices delivery systems.
The published bulletin OMHSAS-26-01 can be found here. Please contact RCPA COO and Mental Health Director Jim Sharp with any questions.
The Office of Mental Health and Substance Abuse Services (OMHSAS) will be hosting their Stakeholder Webinar on Thursday, February 12, 2026, from 3:00 pm – 4:00 pm. Please register for the webinar here. After registering, you will receive a confirmation email containing information about joining the webinar.
For those that want to join via phone:
Call-in Number: +1 (562) 247-8321
Audio Access Code: 385-114-169
The meeting agenda can be found here.