DDAP Awards Nine Grants Totaling $1.2 Million to SCAs for Recovery Housing, Supports for Young Adults
The Pennsylvania Department of Drug and Alcohol Programs (DDAP) is awarding more than $1.2 million to expand access to recovery housing and recovery support services throughout Pennsylvania for young adults 18–24 years old who have opioid or stimulant use disorders. DDAP is awarding grants to nine Single County Authorities (SCA) to fund the effort.
Currently, there are about 430 DDAP-licensed recovery houses across the Commonwealth. The purpose of the Administration’s licensure program is to help empower sustained recovery for individuals with substance use disorder (SUD) by ensuring a network of safe drug and alcohol recovery houses. Drug and alcohol recovery houses are required to be licensed in order to receive referrals from state agencies or state-funded facilities or to receive federal or state funding to deliver recovery house services.
The grant funds will be used to supplement existing resources, ensuring that current services are expanded rather than replaced, and that recovery housing remains accessible and safe through Pennsylvania.
DDAP is awarding nine grants, which will run through September 30, 2026, to the following SCAs serving 14 counties:
- Berks County Council on Chemical Abuse: Berks County
- Blair County Drug and Alcohol Program, Inc.: Blair County
- Columbia Montour Snyder Union Drug & Alcohol Services: Columbia, Montour, Snyder, and Union Counites
- Delaware County Department of Human Services, Division of Drug and Alcohol Programs: Delaware County
- Erie County Office of Drug and Alcohol Abuse: Erie County
- Lackawanna/Susquehanna Office of Drug and Alcohol Programs: Lackawanna and Susquehanna Counties
- Somerset Single County Authority for Drug and Alcohol: Somerset County
- Westmoreland Drug & Alcohol Commission, Inc.: Westmoreland County
- York Adams Drug and Alcohol Commission: York and Adams Counties
Feb. 16 Deadline Nears for SUD Provider Compliance With Final Rule on 42 CFR Part 2: Notice of Privacy Practices
DHS Launches New Website, Shares Inquiry Form for PA Rural Health Transformation Plan
The Department of Human Services (DHS) has launched a new website for the PA Rural Health Transformation Plan, containing information on goals as well as links to the full plan and news updates.
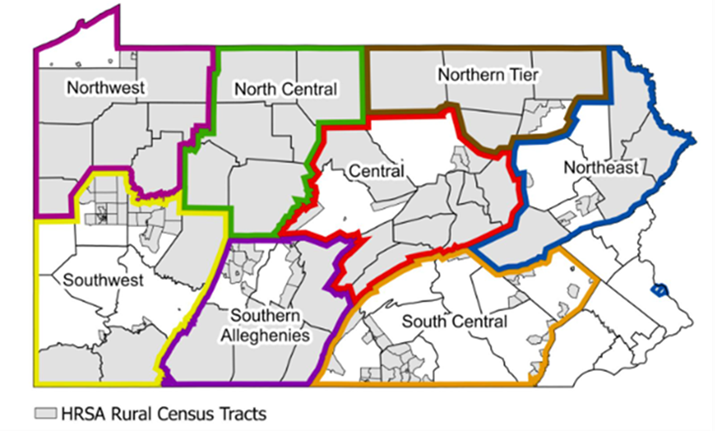
While a formal RFP process has not yet been released, providers can submit the following inquiry form. This brief survey provides each organization with an opportunity to introduce your agency and services you offer, ask questions regarding the Rural Health Transformation Plan, and identify the Rural Care Collaborative region(s) where you and/or your organization is based or provides services (see map below). Once submitted, DHS will review and respond to your inquiry as soon as possible.
Providers and stakeholders may also sign up for updates on the Rural Health Transformation Plan.
If you have any questions, please contact RCPA COO Jim Sharp.
Mental Health Safety Net Coalition Meeting Announced for February 13
RCPA will reengage with all members, non-members, and systems-wide behavioral health stakeholders to participate in the Mental Health Safety Net Coalition. The Coalition is focused on developing strategies, activities, and engagement opportunities to support behavioral health funding in the Commonwealth.
The Coalition will have its first meeting on Friday, February 13, 2026, from 12:00 pm – 1:00 pm. This meeting will give the group an opportunity to review last year’s budget, Governor Shapiro’s proposed budget, and initial strategies for the Fiscal Year (FY) 2026/27. It will also give us an opportunity to develop questions for legislators for the DHS budget hearings in late February and early March. Register for the meeting by contacting Emma Sharp, RCPA Policy Associate.
As the group continues to meet, we will develop our overall advocacy blueprint to ensure the communication of our message and stakeholder engagement is focused on protecting and preserving our mental health service delivery system.
The meetings will be held via Microsoft Teams; information will be sent to those interested in the Coalition. RCPA invites all to participate. If you would like to join the Coalition or have any questions, please contact Emma Sharp.
Free Member Webinar on PA Navigate Announced
CMS Releases Revisions to Telehealth & Remote Monitoring
The Centers for Medicare and Medicaid Services (CMS) recently released a revised Medicare Learning Network (MLN) booklet that contains revisions to telehealth and remote monitoring. Specific changes noted in this publication include:
- The addition of a resource link for the latest telehealth information;
- Additional information on how to suppress a practitioner’s home address in PECOS;
- The removal of telehealth frequency limitations for subsequent inpatient, nursing facility, and critical care consultations;
- Permanently allowing teaching and supervising physicians to supervise through virtual presence;
- Continued payment to Rural Health Clinics (RHC) and Federally Qualified Health Centers (FQHC) for medical telehealth services through December 31, 2026;
- Starting in CY 2026, only adding services to the Medicare telehealth services list on a permanent basis;
- The addition of 5 new CPT and HCPCS codes to the Medicare telehealth services list; and
- For CY 2026, updates to the:
- Medicare Economic Index; and
- Originating site fee.
Members are encouraged to review the booklet for more details on these changes.
Early Bird Rates for NatCon 2026 End Today!
From Chaos to Clarity: The Definitive Client Engagement Case Study — Webinar on January 28 With RCPA Member Qualifacts
From Chaos to Clarity: The Definitive Client Engagement Case Study
Date: Wednesday, January 28, 2026
Time: 12:00 pm CST / 1:00 pm EST
Featuring: Eastern Shore CSB & Qualifacts
Visit Here to Register
Behavioral health organizations are under increasing pressure to do more with less — reduce avoidable rework, improve access to care, and deliver a better client experience without adding staff. In this case-study webinar, Eastern Shore Community Services Board (CSB) shares how they turned fragmented processes into a streamlined, measurable client engagement strategy.
By implementing Qualifacts’ Client Engagement solutions, Eastern Shore CSB modernized intake, communication, and follow-up workflows — keeping care moving, reducing delays, and improving operational clarity across the organization.
Join this webinar to hear directly from the team at Eastern Shore CSB as they walk through what changed, how it changed, and the tangible impact on day-to-day operations.
In this webinar, we will:
- Break down the highest-friction steps in client workflows — including intake, communication, and billing readiness — and show how Eastern Shore standardized them;
- Explore how automated reminders and follow-ups created a consistent client engagement cadence that reduced no-shows and drop-offs;
- Demonstrate how integrated client portal and telehealth workflows expanded access without increasing headcount;
- Show how accelerating signatures and statements in-portal helped maintain billing momentum and avoid downstream delays; and
- Share practical takeaways behavioral health organizations can apply immediately to improve efficiency and client experience.
Featured Speakers
Stephen Hopkins
EHR Systems Administrator, Eastern Shore CSB
Stephen has been with Eastern Shore CSB for eight years and manages all EHR configuration, reporting, virtual care, and client engagement solutions. With a background in Information Technology, he has successfully led the organization’s use of Credible and Credible Client Experience Solutions — driving meaningful improvements in portal adoption, engagement, and telehealth delivery.
Sarah Taylor, RN
Product Specialist II, Qualifacts
Before joining Qualifacts, Sarah spent 16 years as a registered nurse supporting mental health clients across emergency, crisis stabilization, and in-home care settings. She brings hands-on clinical experience and deep implementation expertise to her role, helping organizations maximize the value of Qualifacts’ EHR and client engagement platforms.
Reminder for IPRC Follow-Up Webinar: A Deep Dive Into CARF’s NEW Standards for Disorders of Consciousness

Thursday, January 22, 2026
3:00 pm – 4:00 pm ET; 2:00 pm – 3:00 pm CT;
1:00 pm – 2:00 pm MT; 12:00 pm – 1:00 PT
Register Here
You asked, and we listened! Based on attendee feedback, IPRC is offering a follow-up presentation to pair with the information presented on January 6, 2026. This webinar will provide information on the new Disorders of Consciousness Program Standards in greater detail.
Please join us as IPRC again hosts special guest Terry Carolan from CARF International to explain the new Disorders of Consciousness Program Standards.
Presenter Bio:
Terrence Carolan
Terrence Carolan, Managing Director of the Medical Rehabilitation and Aging Services accreditation areas at the Commission on Accreditation of Rehabilitation Facilities (CARF), has more than 20 years of experience as a provider, administrator, and educator in the human services field. Terry joined CARF after working in clinical and administrative leadership positions within Select Medical’s Inpatient Rehabilitation Division and the Kessler Institute for Rehabilitation since 2001. Terry was a CARF surveyor for 10 years and holds a degree in physical therapy from Simmons College in Boston. He also recently completed his master’s degree in business administration from the University of Wisconsin-Eau Claire.
Objectives: At the end of this session, the learner will:
- Discuss the CARF International Disorders of Consciousness (DoC) Program Standards in detail; and
- Identify the process for applying for Accreditation for a Disorders of Consciousness Specialty Program.
Audience: This webinar is intended for all interested members of the rehabilitation team; attendees do not need to be CARF Certified in order to attend.
Level: Beginner-Intermediate
Certificate of Attendance: Certificates of attendance are available for all attendees. No CEs are provided for this course.