Villanova, PA – December 6, 2023 – Devereux Advanced Behavioral Health, one
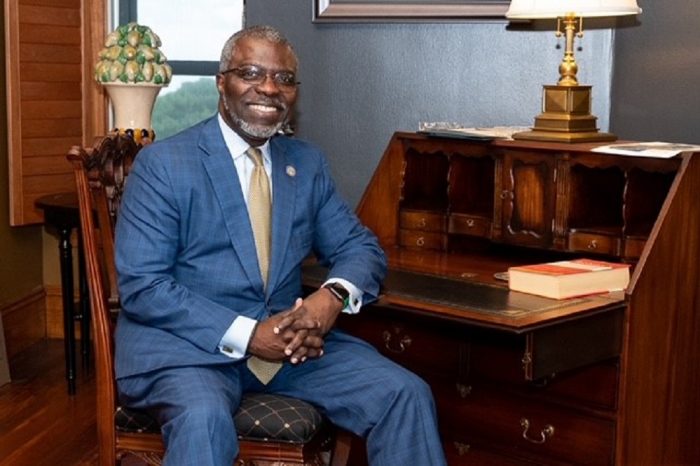
of the nation’s largest nonprofit providers of behavioral healthcare, today announced Clarence D. “Clay” Armbrister has been elected chair of the organization’s National Board of Trustees at the organization’s November meeting.
A trustee since 2013, Armbrister most recently held the role of co-chair of the Board.
“For the past 10 years, Devereux has benefitted from Clay’s expertise in the areas of education, finance, law and government. We also continue to innovate and enhance our programs and services as a result of Clay’s invaluable guidance as a beloved Devereux parent and family member,” said Devereux President and CEO Carl E. Clark II. “His steadfast commitment to our organization – and the individuals and families we serve – is nothing short of inspiring.”
“I look forward to working with Clay in this new capacity to continue advancing our mission and providing the highest quality and most compassionate care for the children, adolescents and adults we support every day,” Clark added.
Devereux requires its National Board of Trustees to include a minimum of five family members, which ultimately helps inform and enrich the Devereux Family Standard. This standard is Devereux’s touchstone principle which demands that, at all times, its programs, practice settings and systems of care match the high levels of quality and compassion of those we would choose for our own family members. Currently, six national Trustees are also Devereux family members.
“I am humbled and honored to be entrusted to help lead an organization that has been so important to our family,” said Armbrister, whose son began receiving educational services through Devereux’s former Kanner Learning Center (now Devereux Pennsylvania Children’s Services) in 1997, and currently receives support from Devereux’s Pennsylvania Adult Services center. “My family and I feel very confident in Devereux, its mission and its future. I will continue to look to my fellow Trustees, and Devereux’s management team, for their leadership and guidance to set and execute the strategic vision for the organization, making sure we deliver on its policies and practices, none of which are more important than the Devereux Family Standard.”
Armbrister assumes the role of chairman of the Board from Christopher D. Butler, who moved into the role of co-chair. “I am incredibly grateful for Chris’ thoughtful and insightful leadership, service and camaraderie during his six years as chairman,” noted Clark. “His vision and outstanding service to our organization have made a significant and positive impact across our entire continuum of care, and I am excited to continue working with Chris as co-chair of our Board.”
About Clarence D. “Clay” Armbrister
Clarence D. “Clay” Armbrister holds more than 40 years of leadership experience across
the private and public sectors. He has served at all levels of education, including senior administrative and leadership positions at several universities and colleges. In addition to his background in education, Armbrister has held executive positions in law, government and finance.
Most recently, Armbrister was the 14th president of Johnson C. Smith University, from 2018 until his retirement in 2023. He began his professional career in 1982 at the Philadelphia law firm of Saul, Ewing Remick & Saul, working his way up to partner. Armbrister left the firm in 1994 to become Philadelphia city treasurer under former Philadelphia Mayor Ed Rendell. From 1996 to 1998, he worked for the Philadelphia School District as managing director, fulfilling the roles of both chief financial officer and chief operating officer, He returned to the private sector in 1999 with PaineWebber (now UBS), advancing to the position of director in the Municipal Securities Group.
Armbrister’s strong belief in the transformative powers of education prompted him to join Temple University in 2003, where he advanced to the position of executive vice president and chief operating officer. From there, he held the following positions in education leadership: senior vice president and chief of staff at Johns Hopkins University (2011), and president of Girard College (2012 to 2018). He also was an adjunct faculty member at Temple University’s Beasley School of Law. In addition, Armbrister served as former Philadelphia Mayor Michael Nutter’s chief of staff, from 2008 to 2011.
Armbrister earned a Bachelor of Arts in political science and economics from the University of Pennsylvania, and a Juris Doctor from the University of Michigan Law School. His long history of board and volunteer service, in addition to Devereux, includes serving on the boards of: Hannon Armstrong Sustainable Infrastructure Capital, Inc. (NYSE: HASI), and Jefferson Health Plans, Inc. Armbrister previously served as board president of the National Adoption Center and a board member of the Community College of Philadelphia. When Armbrister practiced law, he was a member of the following organizations: American Bar Association, National Bar Association, Pennsylvania Bar Association, National Association of Securities Professionals and Government Finance Officers Association.
About Devereux Advanced Behavioral Health
Devereux Advanced Behavioral Health is one of the nation’s largest nonprofit organizations, providing services, insight and leadership in the evolving field of behavioral healthcare. Founded in 1912, Devereux operates a comprehensive national network of clinical, therapeutic, educational and employment programs that positively impact the lives of tens of thousands of children, adults – and their families – every year. The organization’s unique approach combines evidence-based interventions with compassionate family engagement.
With nearly 6,500 employees working in programs across the country, Devereux is a trusted partner for families, schools and communities, serving many of our country’s most vulnerable populations in the areas of autism, intellectual and developmental disabilities, specialty mental health, education and foster care. For more than a century, Devereux Advanced Behavioral Health has been guided by a simple and enduring mission: To change lives by unlocking and nurturing human potential for people living with emotional, behavioral, and cognitive differences.
###











 Charles has led a collaborative data project across 24 Pennsylvania counties. It paints a picture of a devastated workforce.
Charles has led a collaborative data project across 24 Pennsylvania counties. It paints a picture of a devastated workforce.