Justice in Aging Shares Fact Sheet on Impact of HR1 on Older Immigrants’ Access to Health Care


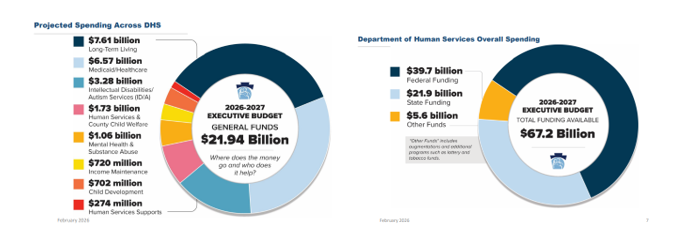
On Friday, February 6, Department of Human Services (DHS) Secretary Val Arkoosh presented an overview of Governor Shapiro’s proposed Fiscal Year (FY) 2026/27 budget and detailed the projected spending across DHS, which totals $21.94 billion in state funding. The Secretary highlighted that all three Medicaid managed care programs, as well as waiver programs for people with intellectual disabilities and autism, are receiving increases, largely driven by patient needs and costs associated with delivering care. The proposed FY 2026/27 budget includes $39.7 billion in federal funding as well as $5.6 billion from augmentations and additional programs, such as lottery and tobacco funds, making the total DHS funding $67.2 billion.
The Secretary expressed how the proposed budget reflects the direct impacts of HR 1, with significant federal funding at risk. The distribution for the 2026/27 budget is based upon the current structure of Medicaid and other federally funded programs, but the Secretary noted that beginning in 2028, changes in Medicaid financing rules will remove $20 billion from Pennsylvania’s Medicaid program over the following decade.
Budget Highlights and Investments
Due to technical difficulties, DHS was unable to record the webinar, but the presentation slides and transcript can both be viewed.
Please contact your RCPA Policy Director with any questions or concerns.
The Pennsylvania Department of Human Services announced that WellKids by RCPA Member PA Health & Wellness will join the network of managed care organizations that offer health coverage through the Children’s Health Insurance Program (CHIP). This marks the first CHIP re-procurement since 2013, expanding the number of affordable health coverage options for children and teens in Pennsylvania. Effective January 2026, CHIP will operate a network of nine managed care organizations, providing comprehensive health coverage for eligible children across the state.
CHIP serves children and teenagers up to age 19 who are not eligible for Medicaid, offering health coverage for free or at a low cost based on family income and providing a variety of insurance plans to best meet a family’s needs. WellKids by PA Health & Wellness will provide a full range of services, including preventative, routine, urgent, and emergency care for physical and behavioral health, as well as coverage for dental, vision, and pharmacy services.
Contact RCPA Policy Associate Emma Sharp with any questions.
Message from the Office of Mental Health and Substance Abuse Services (OMHSAS):
The Pennsylvania Department of Human Services’ (DHS) Office of Mental Health and Substance Abuse Services (OMHSAS) is issuing the bulletin OMHSAS-25-05 “Behavioral Health Clinic Services Provided Outside of the Clinic,” effective November 12, 2025, following changes to Federal Regulation 42 CFR 440.90(d).
OMHSAS 25-05 announces an amendment to Pennsylvania’s Medicaid State Plan which allows all behavioral health clinics that are enrolled in the Medical Assistance (MA) Program, who deliver services through the fee-for-service and managed care systems, to provide clinically appropriate services outside of the clinic. Behavioral health clinics include psychiatric outpatient clinics, outpatient drug and alcohol clinics, and methadone maintenance clinics.
Furthermore, OMHSAS-25-05 also announces the abrogation of 55 Pa Code §§ 1153.14(6) (relating to noncovered services) and 55 Pa. Code 1223.14(11) (relating to noncovered services) by Act 46 of 2025.
The guidance in OMHSAS-25-05 is separate from any “telehealth only” licensure and guidance that may be in place. The changes discussed in this bulletin also do not apply to the existing Mobile Mental Health Telehealth (MMHT) services.
Questions and comments can be directed to OMHSAS via email. RCPA members can also contact RCPA COO and MH Policy Director Jim Sharp with any questions.
The Pennsylvania Department of Human Services’ (DHS) Office of Mental Health and Substance Abuse Services (OMHSAS) and the Office of Medical Assistance Programs (OMAP) have jointly issued the Medical Assistance Bulletin Targeted Case Management Services for Eligible Juveniles Enrolled in Medical Assistance Prior to Release From a Carceral Setting, implementing Section 5121 of the Consolidated Appropriations Act, 2023. Eligible juveniles are individuals under 21 years of age who are determined eligible for MA or an individual 18–25 years of age who was determined eligible for the mandatory eligibility group for former foster care children.
This bulletin advises providers of billing procedures for the physical health (PH) and behavioral health (BH) Targeted Case Management (TCM) services provided to eligible juveniles enrolled in the Medical Assistance (MA) Program within 30 days of release from a carceral setting and for at least 30 days following release. This bulletin also advises providers of a new provider specialty (Spec) for TCM services.
Questions and comments can be sent electronically. You can also contact RCPA Policy Associate Emma Sharp with any questions.
From Pennsylvania Capital-Star “Pa.’s Rural Health Application Reveals Priorities in Federal Funding Request,” November 20, 2025:
Pennsylvania is hoping to secure its own slice of a $50 billion rural health fund in the face of federal Medicaid cuts, with a focus on bolstering a beleaguered workforce and expanding health access for more than two million people.
The Rural Health Transformation Fund was a last-minute addition to President Donald Trump’s summer budget bill that imposed Medicaid work requirements and cut upwards of $51 billion in funding to the commonwealth over the next decade. That new fund is worth roughly 37% of the estimated lost Medicaid funding in rural areas…
The 67-page application requests up to $200 million in annual funding over the next five years, totaling $1 billion. Its six focuses include: technology and infrastructure, workforce, maternal health services, behavioral health services, aging and access, and emergency medical services and transportation.
The U.S. Department of Human Services is expected to award funding by the end of the year.
Key objective targets are:
From the PA Rural Health Transformation (RHT) Program Application:
Pennsylvania’s rural health transformation strategy is grounded in a balance of statewide coordination and regional leadership and collaboration. Pennsylvania’s “Health Hub” state agencies (Human Services, Health, Aging, Insurance, Drug and Alcohol Programs), and other partner agencies will establish clear strategic priorities focusing on access, workforce, maternal health, aging, behavioral health, EMS and infrastructure. Pennsylvania will leverage statewide technical expertise, evaluation, and financial oversight and support. Strong regional rural care collaborative will be composed of a roster of regional stakeholders that prioritize local needs, develop effective local sustainable solutions, and leverage existing resources and assets.
Pennsylvania will leverage established regional entities that coordinate regional economic development. These Partnerships for Regional Economic Performance (PREP) organizations are long-standing, quasi-governmental organizations that convene regional stakeholders, administer federal and state grants, collect local data, report outcomes, and catalyze public and private partnerships for regional economic development. They bring established governance structures, convening power, and a track record of successful cross-sector collaboration. PREPs (Figure 2) will convene regional stakeholders to create Rural Care Collaborative (RCCs) to align initiatives with regional economic planning and development – making the RHTP investments sustainable and promoting long-term partnerships.
If you have any questions, please contact RCPA COO and Mental Health Policy Director Jim Sharp.