From Pennsylvania Capital-Star “Pa.’s Rural Health Application Reveals Priorities in Federal Funding Request,” November 20, 2025:
Pennsylvania is hoping to secure its own slice of a $50 billion rural health fund in the face of federal Medicaid cuts, with a focus on bolstering a beleaguered workforce and expanding health access for more than two million people.
The Rural Health Transformation Fund was a last-minute addition to President Donald Trump’s summer budget bill that imposed Medicaid work requirements and cut upwards of $51 billion in funding to the commonwealth over the next decade. That new fund is worth roughly 37% of the estimated lost Medicaid funding in rural areas…
The 67-page application requests up to $200 million in annual funding over the next five years, totaling $1 billion. Its six focuses include: technology and infrastructure, workforce, maternal health services, behavioral health services, aging and access, and emergency medical services and transportation.
The U.S. Department of Human Services is expected to award funding by the end of the year.
Key objective targets are:
- Access to care: More than 85% of Pennsylvanians can get a routine primary care appointment within four weeks and urgent care appointments within one week.
- Digital connectivity and telehealth: More than 85% of rural hospitals and clinics will have broadband and telehealth functionality. More than 50% of rural hospitals and clinics connected via Fast Healthcare Interoperability Resources.
- Workforce adequacy: Reduce rural hospital vacancy rates by 10% for key direct care roles. Add three new rural training programs.
- System sustainability: More than 60% of systems partnered with rural Community Health Centers for specialty care.
- Health outcomes: Reduce the number of pregnant women living in rural areas with inadequate prenatal care by 20%.
From the PA Rural Health Transformation (RHT) Program Application:
Pennsylvania’s rural health transformation strategy is grounded in a balance of statewide coordination and regional leadership and collaboration. Pennsylvania’s “Health Hub” state agencies (Human Services, Health, Aging, Insurance, Drug and Alcohol Programs), and other partner agencies will establish clear strategic priorities focusing on access, workforce, maternal health, aging, behavioral health, EMS and infrastructure. Pennsylvania will leverage statewide technical expertise, evaluation, and financial oversight and support. Strong regional rural care collaborative will be composed of a roster of regional stakeholders that prioritize local needs, develop effective local sustainable solutions, and leverage existing resources and assets.
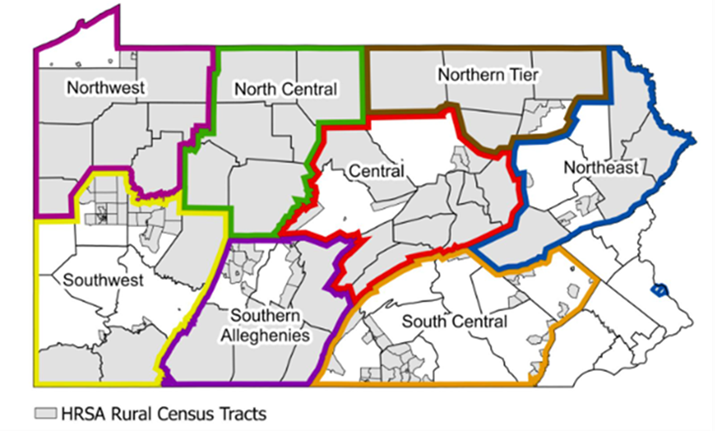
Pennsylvania will leverage established regional entities that coordinate regional economic development. These Partnerships for Regional Economic Performance (PREP) organizations are long-standing, quasi-governmental organizations that convene regional stakeholders, administer federal and state grants, collect local data, report outcomes, and catalyze public and private partnerships for regional economic development. They bring established governance structures, convening power, and a track record of successful cross-sector collaboration. PREPs (Figure 2) will convene regional stakeholders to create Rural Care Collaborative (RCCs) to align initiatives with regional economic planning and development – making the RHTP investments sustainable and promoting long-term partnerships.
If you have any questions, please contact RCPA COO and Mental Health Policy Director Jim Sharp.