Jim Sharp
Harrisburg Area Transportation Study (HATS) Shares Capital Region Mobility Plan Survey
CHCS Shares Federal Rural Health Transformation Plan Resources

RCPA has been a long-time partner of the Center for Health Care Strategies (CHCS), a policy design and implementation organization devoted to improving outcomes for people enrolled in Medicaid. Our collaborative efforts across the arena of Medicaid and the pending impacts of HR 1 remain a critical connection point to ensure access in Pennsylvania.
On behalf of CHCS, RCPA would like to share this update on resources related to the Rural Health Transformation Project. Per the update:
The federal Rural Health Transformation Program (RHTP), authorized under the 2025 budget reconciliation act (P.L. 119-21), will distribute $50 billion to all 50 states from 2026 to 2030 — serving as a partial offset to Medicaid cuts. In designing and launching RHTP plans, state agencies must meet ambitious federal expectations and timelines. Experiences from other large-scale statewide efforts — such as the American Rescue Plan Act, Opioid Settlement Funds, multisector plans for aging (MPA), and the Centers for Medicare & Medicaid Services’ (CMS) State Innovation Models (SIM) demonstration — can help inform state planning.
This brief provides practical recommendations to help states establish the administrative infrastructure needed to implement their RHTP plans. Drawing on insights from state officials involved with similar transformation efforts, as well as the Center for Health Care Strategies’ (CHCS) experience supporting this work, the brief highlights best practices and common pitfalls across four core domains:
- Governance;
- Stakeholder engagement and communications;
- Budget tracking, reporting, and contracting; and
- Data and evaluation.
While not exhaustive, this brief outlines practical lessons that state staff can use to guide RHTP activities during the critical first six to nine months of program design and implementation, helping states build a strong foundation for long-term success.
Additionally, CHCS published a series of tip sheets to aid stakeholders in exploring strategies and initiatives within the project. The tip sheets offer resources for strengthening rural health, including workforce and access issues.
If members have any questions regarding this update or the Rural Health Transformation Plan, please contact RCPA COO Jim Sharp.
OCDEL EI Training on DC:0-5 MH Diagnostic Classifications Announced
With support from the Preschool Development Grant, the Office of Child Development and Early Learning (OCDEL) is supporting a training initiative to help build a cross-disciplinary workforce across Pennsylvania that understands very young children’s mental health and development and can provide better, more informed support to families and caregivers.
You, or a Children First PA representative(s) of your choosing, are invited to participate in an upcoming DC:0–5™: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood Overview webinar. This 90-minute session is designed for policy leaders, advocates, and human services administrators who play a pivotal role in shaping systems that support the mental health and well-being of our youngest children.
About the Training:
The DC:0–5™ framework provides a developmentally sensitive approach to understanding and classifying mental health and developmental disorders in children from birth through age five. The overview will:
- Introduce the purpose and structure of the DC:0–5™;
- Highlight its role in transforming early identification and intervention practices; and
- Explore implications for policy, advocacy, and service delivery.
Why Your Participation Matters:
Your leadership and expertise are essential in ensuring that policies and programs reflect the latest understanding of infant/early childhood mental health. By engaging in this training, you will be better equipped to:
- Inform policy decisions with evidence-based practices;
- Strengthen cross-sector collaboration; and
- Support equitable access to infant/early childhood mental health services and supports.
DATE: February 18, 2026, from 2:00 pm – 3:30 pm EST
Participants will need to create a free eLearn account with ZERO TO THREE if they do not already have one to complete their registration.
Priority registration is available through February 11, 2026, before the training announcement is made public the following day. Space is limited to 100 attendees.
We look forward to your participation in this important conversation and to working together to advance the well-being of young children and their families. If you cannot attend this session, there will be additional opportunities in 2027, as this initiative also includes a Training of Trainers strategy.
If you have any additional questions, please contact RCPA COO Jim Sharp.
RCPA IDD Policy Director Tim Sohosky Honored for Commitment to Public Education
Workplace Violence & Safety Bootcamp Offered by RCPA Member Conner Strong & Buckelew Feb. 19
Senate Passes FY26 Funding for Mental Health and SUD
From our partners at the National Council on Mental Wellbeing:
After a brief partial shutdown on Feb. 3, Congress passed an amended funding package that includes funding for five appropriations bills; the package now goes to the president’s desk for signature. The package also includes a two-week continuing resolution to temporarily fund the Department of Homeland Security (DHS) while a longer term deal is negotiated. If no funding deal is reached for DHS within the two-week timeframe, it is possible another partial shutdown will occur; however, Health and Human Services (HHS) programs would not be impacted.
Funding for HHS is included in the final fiscal year (FY) 2026 funding for the Labor, Health and Human Services, Education, and Related Agencies (LHHS) bill. See the Consolidated Appropriations Act, 2026 bill text and its accompanying report language.
Total funding for the Substance Abuse and Mental Health Services Administration (SAMHSA) was provided at $7.4 billion, relatively level to funding provided in FY24, when appropriations bills were last enacted (FY25 saw a year-long continuing resolution rather than an appropriations bill).
Overall, many mental health and substance use programs saw level or slightly increased funding. This is a tremendous win for the field, particularly in a challenging fiscal environment.
The Medicare telehealth waivers expired on January 30, 2026; and after a brief lapse in the telehealth waivers and a partial shutdown of the federal government, this passage restores continuity to Medicare telehealth coverage and a return to permanent, pre-pandemic policy. The extension will maintain key flexibilities, including expanded originating sites, geographic waivers, and eligibility for certain providers that would otherwise be unavailable under permanent Medicare telehealth rules. Additionally, this will apply retroactively and cover the lapse period for the delivery and billing of these services.
Additional language in the agreement includes a requirement that the Department of Health and Human Services (HHS) notify the committee at least three days prior to announcing or providing notice of a grant termination and directs SAMHSA to consult with Congress before issuing a funding opportunity announcement. This language provides additional congressional oversight in the agency grant making process. If you have any questions, please contact RCPA COO & Mental Health Division Director Jim Sharp.
Governor Shapiro to Deliver 2026/27 Proposed Budget Today
Today, February 3, Pennsylvania Governor Josh Shapiro is set to deliver his 2026/27 proposed budget to the PA General Assembly with the backdrop of ongoing concerns regarding looming funding cuts at both the Federal and State levels. RCPA will cover the presentation and work to provide a global overview of the Governor’s budget design, as well as areas that may impact members, by COB today. Throughout the week, RCPA Policy Directors will be conducting a deeper review of the impacts, as well.
Additionally, we understand DHS Secretary Dr. Valerie Arkoosh will give a webinar later in the week to present the DHS specifics in the proposed plan. As details become available, RCPA will communicate the information to members.
Governor Shapiro’s budget presentation is set to begin at 11:30 am and can be watched through the following streaming links:
If you have any questions, please contact your respective RCPA Policy Director.
DHS Launches New Website, Shares Inquiry Form for PA Rural Health Transformation Plan
The Department of Human Services (DHS) has launched a new website for the PA Rural Health Transformation Plan, containing information on goals as well as links to the full plan and news updates.
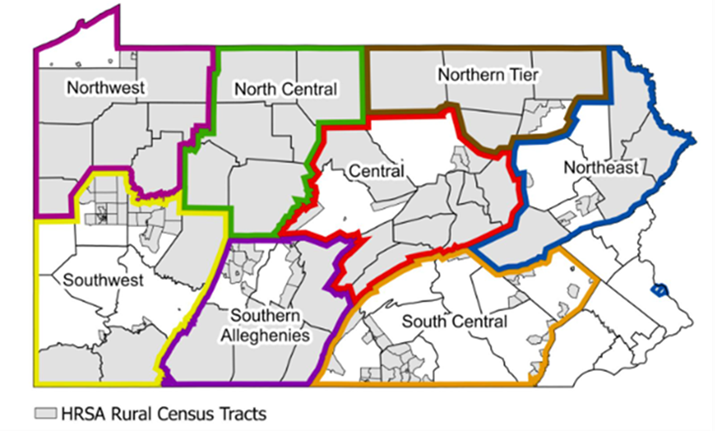
While a formal RFP process has not yet been released, providers can submit the following inquiry form. This brief survey provides each organization with an opportunity to introduce your agency and services you offer, ask questions regarding the Rural Health Transformation Plan, and identify the Rural Care Collaborative region(s) where you and/or your organization is based or provides services (see map below). Once submitted, DHS will review and respond to your inquiry as soon as possible.
Providers and stakeholders may also sign up for updates on the Rural Health Transformation Plan.
If you have any questions, please contact RCPA COO Jim Sharp.

















