The Department of Defense (DoD) issued a proposed rule to add certified or licensed physical therapy assistants (PTAs) and occupational therapy assistants (OTAs) as TRICARE-authorized providers, to engage in physical or occupational therapy, under the supervision of a TRICARE-authorized physical or occupational therapist, in accordance with Medicare’s rules for supervision and qualification when billed by under the supervising therapist’s national provider identification number. This rule will align TRICARE with Medicare’s policy. Comments on this proposed rule will be accepted until Tuesday, February 19, 2019. Contact Melissa Dehoff, RCPA Director of Rehabilitation Services, with questions.
Melissa Dehoff
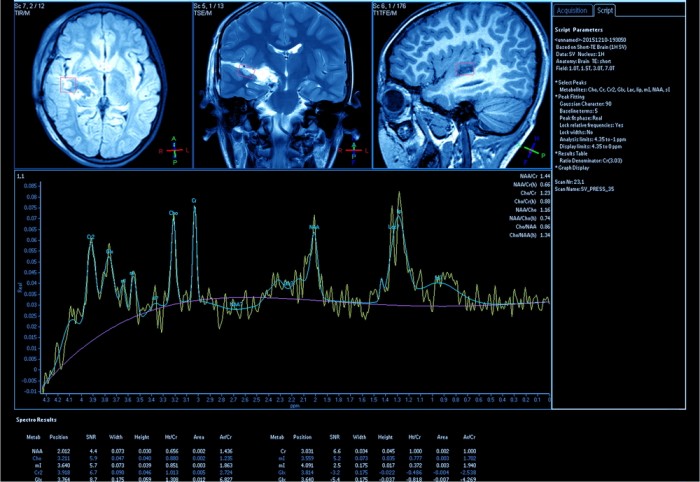
Head Injury Program Accepting Applications for Individuals 18 & Older
The Pennsylvania Department of Health (DOH) published a notice in the January 26, 2019 Pennsylvania Bulletin indicating that effectively immediately, they will begin accepting applications to the Head Injury Program (HIP) for individuals 18 years of age and older.
The HIP, administered in the Bureau of Family Health (BFH), through the Emergency Medical Services Act of 1985, funds short-term intensive brain injury rehabilitation for residents in this Commonwealth who have sustained a traumatic brain injury.
To provide these services, the HIP contracts with specialized brain injury providers who offer therapies such as physical, occupational, speech, and cognitive therapies, along with assistive community integration and psychological services. Rehabilitation services can be received in a residential setting as outpatient services or as home-based and community-based services depending on the need of the individual.
To obtain an application, contact the HIP at 717-772-2763 or the Brain Injury Helpline at 866-412-4755.
OLTL Definition of Day Unit Survey for Residential Habilitation Providers
Today, the Office of Long-Term Living (OLTL) issued a survey to all residential habilitation providers to obtain information regarding 2017 utilization and the definition of a day unit. The link to the survey is below and all residential habilitation providers are strongly encouraged to complete it.
This issue is one that the brain injury providers have been asking OLTL to address and change for years. Fewer responses to this survey will prevent Mercer from having sufficient data to estimate the cost associated with making the change to the service definition that the Centers for Medicare and Medicaid Services (CMS) requires when requesting an amendment.
The responses to the survey are due by February 22, 2019. Please do not delay and respond today!
Please contact Mike Penney at OLTL if you have any issues completing the survey.
CHC Third Thursday Webinar Scheduled for Jan 17
The next Community HealthChoices (CHC) Third Thursday webinar has been scheduled for January 17, 2019, 1:30 pm – 3:00 pm. Some of the agenda topics to be included during this webinar include updates from Deputy Secretary Kevin Hancock on the initial CHC implementation efforts in the Southeast; and Randy Nolen will lead a discussion on launch indicators and Operations Reports data. In addition, the Office of Long-Term Living (OLTL) Chief Medical Officer, Dr. Lawrence Appel, will present on quality activities and performance measures in the Southwest from the first year of CHC.
To participate in the webinar, participants need to register. After participants register, a confirmation email will be sent containing information about joining the webinar.
Questions should be directed to the OLTL Bureau of Policy and Regulatory Management at 717-857-3280.
OLTL Issues Billing Clarification for Cog Rehab Therapy
The Office of Long-Term Living (OLTL) issued a billing clarification for Cognitive Rehabilitation Therapy (CRT) Procedure Code 97127 SE.
This procedure code can be billed by either billing each date of service separately per claim or by billing each date of service on separate detail lines of a date spanned claim.
Examples:
Billing each date of service separately per claim:
Would mean billing each date of service for each recipient for this procedure code individually. Each date is recognized as a new claim and will have a different ICN.
Billing each date of service on separate detail lines of a date spanned claim:
Would mean span dating the dates of service from one date to another date. At the bottom of the claims each date of service is a different line or number. This will show each day on a different line in the detail section of the claim.
Providers should continue to use the SE modifier per the OLTL fee schedule.
Questions regarding this clarification should be directed to the OLTL Provider Inquiry Unit via email or 800-932-0939.
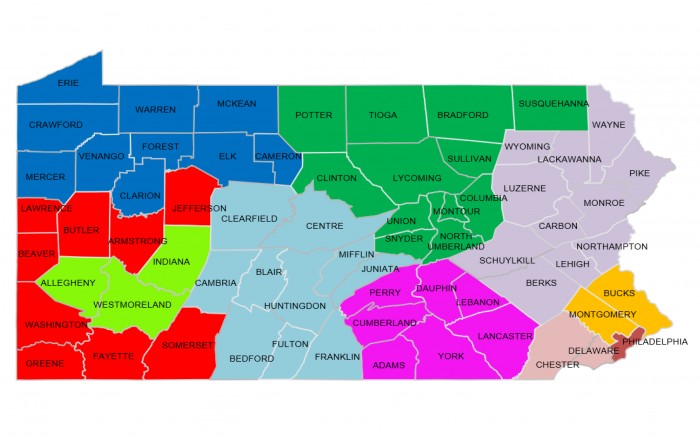
PA IEB Outreach Coordinator Contacts & Maps
The Community Relations Manager for the Pennsylvania Independent Enrollment Broker (IEB) program (aka Maximus) has provided a map of Outreach Coordinators on the team and their coverage areas. This information was requested during the December 19, 2018 RCPA Physical Disabilities and Aging Division meeting.
Please Note: Jennifer Borgess in the North Central Region (shown in green on the map) is leaving the PA IEB (her last day will be January 4, 2019). Until a replacement is found for this region, if someone in that region reaches out to the PA IEB, please copy Joan Landis (Community Relations Manager) and Jahd Burns (her team supervisor) to ensure the issue is addressed by someone. Once a new coordinator in that area is hired and trained to take over this region, an updated map will be issued.
Contact Melissa Dehoff, RCPA Rehabilitation Services Director, with questions.
CMS Issues Clarification on Role of Therapy Students in IRFs
During the November Centers for Medicare and Medicaid Services (CMS) National Provider call with inpatient rehabilitation facilities (IRFs), CMS responded to a question related to the counting of minutes of therapy provided by a therapy student that these minutes would not count, regardless of the level of supervision.
This triggered much confusion and led to the therapy professional associations requesting a meeting with CMS to discuss and address this and their concerns surrounding this response. After this collaborative effort between these associations and CMS, CMS issued a clarification of its position on therapy students in IRFs.
CMS has noted that student therapists may participate in therapy provided in an IRF if the student is appropriately supervised, and that the time spent with the student may count towards satisfying intensity of therapy requirements for IRFs. Cited directly from the clarification:
“Regarding the IRF intensive rehabilitation therapy program requirement in 42 CFR 412.622(a)(3)(ii), CMS’s current policy does not prohibit the therapy services furnished by a therapy student under the appropriate supervision of a qualified therapist or therapy assistant from counting toward the intensive rehabilitation therapy program. However, IRFs provide a very intensive hospital level of rehabilitation therapy to some of the most vulnerable patients. To ensure the health and safety of this vulnerable population, CMS expects that all student therapy services will be provided by students under the supervision of a licensed therapist allowed by the hospital to provide such services.”
Contact Melissa Dehoff, RCPA Rehabilitation Services Director, with questions.
CMS Issues KX Modifier Thresholds/Related Policy Updates for CY 2019
The Centers for Medicare and Medicaid Services (CMS) released Change Request (CR) 11055, “Annual Update to the Per-Beneficiary Therapy Amounts.” This CR provides information on the annual per-beneficiary incurred expense amounts, now known as the KX modifier thresholds, and related policy updates for calendar year (CY) 2019. These amounts were previously associated with the financial limitation amounts (therapy caps) before the application of the therapy caps was repealed when the Bipartisan Budget Act (BBA) of 2018 was signed into law.
For CY 2019, the KX modifier threshold amount for physical therapy (PT) and speech-language pathology (SLP) services combined is $2,040. For occupational therapy (OT) services, the CY 2019 threshold amount is $2,040.
Contact Melissa Dehoff, RCPA Rehabilitation Services Director, with questions.
Senate Committee Reauthorizes TBI Program
The United States Senate Committee on Health, Education, Labor & Pensions (HELP) recently held an executive session and voted to advance S.3657 – the Traumatic Brain Injury Program Reauthorization Act of 2018. The bill included some increased funding (from $5,500,000 to $7,321,000 for 2020 through 2014) and reauthorized the Traumatic Brain Injury (TBI) State Partnership Grant Program, which is administered by the Administration for Community Living (ACL).
The bill also created and funded a national concussion data collection and analysis program through the Centers for Disease Control and Prevention (CDC) to determine the prevalence and incidence of concussion. Contact Melissa Dehoff, RCPA Director of Rehabilitation Services, with questions.
IRF National Provider Call Recording & Transcript Available
On November 15, 2018, the Centers for Medicare and Medicaid Services (CMS) held a National Provider Call for inpatient rehabilitation facilities (IRFs) that focused on the changes included in the fiscal year (FY) 2019 inpatient rehabilitation facility prospective payment system (IRF PPS) final rule.
CMS has posted the presentation from this call and recently posted both the audio recording and transcript. RCPA encourages all members in the Rehabilitation Services Division to listen to this recording or read the transcript from this call. Questions can be directed to Melissa Dehoff.