Important COVID-19 Guidance for Behavioral Health Residential Facilities
Westmoreland County Blind Association Manufacturing Face Masks
Civil Rights Complaint Filed by Disability Rights PA Resulted in Progress on Medical Rationing Guidelines
In response to a civil rights complaint filed by Disability Rights Pennsylvania (DRP) and other advocacy groups, the U.S. Department of Health & Human Services’ Office for Civil Rights (OCR) announced on April 16, 2020, that Pennsylvania has made changes to its proposed guidelines on rationing of scarce medical care resources needed to treat COVID-19 patients that better protect people with disabilities from discrimination. Guidelines can be found here.
DOH removed criteria that automatically deprioritized persons needing critical care on the basis of particular disabilities and has included language to ensure that no one will be denied care based on stereotypes, assessments of quality of life, or judgments about a person’s “worth” based on disabilities. Importantly, OCR cautioned that “[t]his result does not, however, preclude future OCR enforcement in cases of potential discriminatory implementation of Pennsylvania’s policies by any covered health care provider.”
The Guidelines include the following protections for people with disabilities:
- No categorical exclusions. No person will be disqualified from receiving critical care solely on the basis of their disability. Health care providers cannot use a list of disabilities to de-prioritize those patients for critical care if rationing is implemented. As the Guidelines explain, such exclusions “will make many feel like their lives are ‘not worth saving,’ leading to justified perceptions of discrimination.”
- A prohibition on reallocation of the personal ventilators that adults with disabilities ordinarily use and bring with them when they seek care.
- No reference to specific disabilities as a basis to reduce the likelihood that those individuals would receive critical care.
- No consideration of life expectancy in the longer term, including 10-year life expectancy after critical care treatment.
- No one can “be denied care based on stereotypes, assessments of quality of life or judgments about a person’s ‘worth’ based on the presence or absence of disabilities or other factors.”
- All rationing decisions must be based on individualized patient assessments by clinicians using the best available objective medical evidence. This means that rationing decisions cannot be based on discriminatory assumptions about a person’s disability or medical condition.
- “Triage officers” – the health care professionals who will be responsible to make any rationing decisions – should receive training on implicit bias and cultural competency.
- Patients and their family members or caregivers who have concerns about rationing decisions should be notified of their right to express their concerns or file a complaint with the hospital. Unresolved or unsatisfactorily resolved complaints can be brought to the Pennsylvania Department of Health.
While the above changes go a long way in ensuring that people with disabilities do not suffer from discrimination, DRP remains concerned about a number of the Guidelines’ principles:
First, in rationing care, the Guidelines allow health care providers to consider predictions about how long a person will live in the short term, including up to five years after treatment, due to a disability or medical condition unrelated to COVID-19. This rule could unfairly limit access to health care resources for people with disabilities. To avoid discrimination, health care providers should only consider a person’s immediate term survivability, that is, the likelihood of surviving COVID-19 if provided treatment.
Second, the Guidelines do not explicitly instruct health care providers that they are required under the law to make reasonable modifications to accommodate people with disabilities, including by:
- Making modifications to the assessment tools used under the Guidelines if a person cannot be accurately and fairly assessed due to a disability.
- Making modifications for people whose disabilities might require a longer period of treatment – for example, on a ventilator – in order to ensure an equal opportunity to benefit from the treatment.
- Providing effective communication to people with sensory disabilities and making modifications to restrictive visitor policies to allow individuals with disabilities who need family members or staff to accompany them in the hospital to ensure that they are properly assessed and can participate in their treatment.
To continue to advocate for the rights of people with disabilities on this issue, DRP is opening a Health Care Rationing Hotline during the pandemic. Individuals with disabilities or family members or caregivers of individuals with disabilities who experience discrimination in health care rationing, who are denied effective communication at the hospital, or who are prohibited from bringing a needed family member or staff with them in the hospital should contact DRP at 1.800.692.7334 ext 402.
DRP has also created a fact sheet to assist people with disabilities with questions or concerns about medical rationing. It can be found here.
Gov. Wolf Unveils Plan for Pennsylvania’s COVID-19 Recovery
Joint Letter to Congress Regarding Additional Legislative Requests to Respond to COVID Pandemic
On Wednesday, April 15, ADvancing States and the National Association of State Directors of Developmental Disabilities Services (NASDDDS) sent a letter to Congress outlining additional legislative requests to assist state aging, disability, and LTSS agencies as they respond to the COVID pandemic. Specifically, the letter requests:
- Further increase the Medicaid Federal Medical Assistance Percentage (FMAP) to a total of 12%;
- Allow states to provide Medicaid retainer payments to additional provider categories and for extended periods of time as warranted by the emergency;
- Provide additional supports to ensure that older adults and people with disabilities have access to food;
- Delay the CURES Act Electronic Visit Verification penalties;
- Delay the proposed Medicaid Financial Accountability Regulation (MFAR); and
- Provide additional resources for Adult Protective Services to respond to abuse, neglect, and exploitation.
Click here to read the full letter.
CMS Releases IRF PPS Proposed Rule for FY 2021
The Centers for Medicare and Medicaid Services released the inpatient rehabilitation facility prospective payment system (IRF PPS) proposed rule for fiscal year (FY) 2021. Due to the COVID-19 public health emergency and the demands that have been placed on the healthcare industry, CMS limited the rulemaking to essential policies and proposals to reduce provider burden and assist IRF’s, especially in the COVID-19 response. Some of the proposals include:
- Payment: CMS proposes to implement its annual updates to the weights and average lengths of stays for the IRF PPS Case Mix Groups (CMGs), update the standard payment conversion factor due to growth in the IRF market basket, and increase the labor-related share. Overall, CMS estimates payments to IRFs will increase by 2.9 percent.
- IRF Coverage Requirements: CMS proposes to amend the IRF coverage requirements to remove the post-admission physician evaluation (PAPE) requirement.
- Non-Physician Practitioners: CMS proposes to modify the IRF coverage requirements to allow non-physician practitioners (NPP) to perform certain services that are currently required to be performed by a rehabilitation physician. Some of these services include the pre-admission screening, developing the individual plan of care, performing three face-to-face visits per week, and leading interdisciplinary team meetings
- Documentation: CMS proposes to codify existing documentation instructions and guidance to ensure uniformity between the Medicare Benefit Policy Manual and regulations that are applicable.
- Definition of a Week: CMS clarifies that, for the purposes of the intensity of therapy requirement, a “week” would be defined as a period of seven consecutive calendar days beginning with the date of admission to the IRF.
- Quality Reporting Program (QRP): The only provision impacting the QRP in the proposed rule is a two percent reduction to the applicable FY 2021 market basket increase factor for IRFs that fail to comply with quality data submission requirements.
- Outlier Threshold: CMS proposes to update the outlier threshold amount from $9,300 for FY 2020 to $8,102 for FY 2021 ensure outlier payments account for 3 percent of total payments. CMS estimates there will be a $40 million increase in aggregate payments to IRFs due to this proposed change. The outlier threshold is used to determine when an IRF is entitled to an outlier payment. CMS attempts to set the outlier threshold each year so that 3 percent of total payments are outliers.
The proposed rule will be published in the April 21, 2020 edition of the Federal Register. A more in-depth analysis will be forthcoming following the publication. A fact sheet is also available for members to obtain additional information.
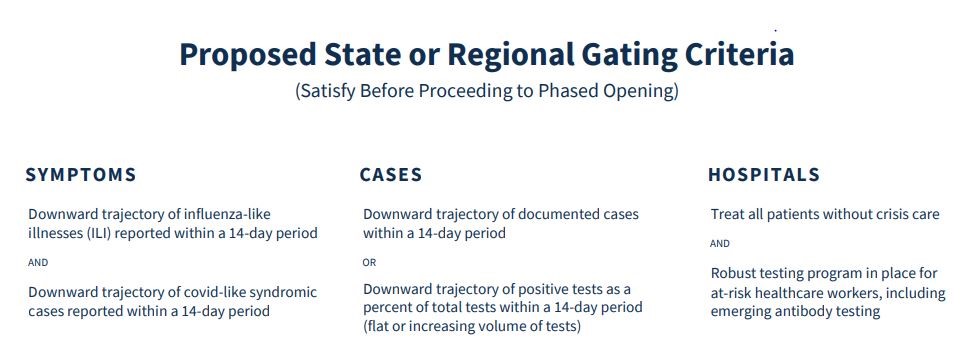
President Trump Announces Guidelines for Opening Up American Economy
President Trump Announces Guidelines for Opening Up American Economy
FOR IMMEDIATE RELEASE
April 16, 2020
U.S. PRESIDENT, DONALD TRUMP: Guidelines Opening Up America Again
PHASE 1:
INDIVIDUALS
- ALL VULNERABLE INDIVIDUALS* should continue to shelter in place. Members of households with vulnerable residents should be aware that by returning to work or other environments where distancing is not practical, they could carry the virus back home. Precautions should be taken to isolate from vulnerable residents.
- All individuals, WHEN IN PUBLIC (e.g., parks, outdoor recreation areas, shopping areas), should maximize physical distance from others. Social settings of more than 10 people, where appropriate distancing may not be practical, should be avoided unless precautionary measures are observed.
- Avoid SOCIALIZING in groups of more than 10 people in circumstances that do not readily allow for appropriate physical distancing (e.g., receptions, trade shows)
- MINIMIZE NON-ESSENTIAL TRAVEL and adhere to CDC guidelines regarding isolation following travel.
EMPLOYERS
- Continue to ENCOURAGE TELEWORK, whenever possible and feasible with business operations. If possible, RETURN TO WORK IN PHASES.
- Close COMMON AREAS where personnel are likely to congregate and interact, or enforce strict social distancing protocols.
- Minimize NON-ESSENTIAL TRAVEL and adhere to CDC guidelines regarding isolation following travel.
- Strongly consider SPECIAL ACCOMMODATIONS for personnel who are members of a VULNERABLE POPULATION.
SPECIFIC TYPES OF EMPLOYERS
- SCHOOLS AND ORGANIZED YOUTH ACTIVITIES (e.g., daycare, camp) that are currently closed should remain closed.
- VISITS TO SENIOR LIVING FACILITIES AND HOSPITALS should be prohibited. Those who do interact with residents and patients must adhere to strict protocols regarding hygiene.
- LARGE VENUES (e.g., sit-down dining, movie theaters, sporting venues, places of worship) can operate under strict physical distancing protocols.
- ELECTIVE SURGERIES can resume, as clinically appropriate, on an outpatient basis at facilities that adhere to CMS guidelines.
- GYMS can open if they adhere to strict physical distancing and sanitation protocols. BARS should remain closed.
PHASE 2: FOR STATES AND REGIONS WITH NO EVIDENCE OF A REBOUND AND THAT SATISFY THE GATING CRITERIA A SECOND TIME
INDIVIDUALS
- ALL VULNERABLE INDIVIDUALS should continue to shelter in place. Members of households with vulnerable residents should be aware that by returning to work or other environments where distancing is not practical, they could carry the virus back home. Precautions should be taken to isolate from vulnerable residents.
- All individuals, WHEN IN PUBLIC (e.g., parks, outdoor recreation areas, shopping areas), should maximize physical distance from others.
- Social settings of more than 50 people, where appropriate distancing may not be practical, should be avoided unless precautionary measures are observed.
- NON-ESSENTIAL TRAVEL can resume.
EMPLOYERS
- Continue to ENCOURAGE TELEWORK, whenever possible and feasible with business operations.
- Close COMMON AREAS where personnel are likely to congregate and interact, or enforce moderate social distancing protocols.
- NON-ESSENTIAL TRAVEL can resume.
- Strongly consider SPECIAL ACCOMMODATIONS for personnel who are members of a VULNERABLE POPULATION.
SPECIFIC TYPES OF EMPLOYERS
- SCHOOLS AND ORGANIZED YOUTH ACTIVITIES (e.g., daycare, camp) can reopen.
- VISITS TO SENIOR CARE FACILITIES AND HOSPITALS should be prohibited. Those who do interact with residents and patients must adhere to strict protocols regarding hygiene.
- LARGE VENUES (e.g., sit-down dining, movie theaters, sporting venues, places of worship) can operate under moderate physical distancing protocols.
- ELECTIVE SURGERIES can resume, as clinically appropriate, on an outpatient and in-patient basis at facilities that adhere to CMS guidelines.
- GYMS can remain open if they adhere to strict physical distancing and sanitation protocols.
- BARS may operate with diminished standing-room occupancy, where applicable and appropriate.
PHASE THREE: FOR STATES AND REGIONS WITH NO EVIDENCE OF A REBOUND AND THAT SATISFY THE GATING CRITERIA A THIRD TIME
INDIVIDUALS
- VULNERABLE INDIVIDUALS can resume public interactions, but should practice physical distancing, minimizing exposure to social settings where distancing may not be practical, unless precautionary measures are observed.
- LOW-RISK POPULATIONS should consider minimizing time spent in crowded environments.
EMPLOYERS
- Resume UNRESTRICTED STAFFING of worksites.
SPECIFIC TYPES OF EMPLOYERS
- VISITS TO SENIOR CARE FACILITIES AND HOSPITALS can resume. Those who interact with residents and patients must be diligent regarding hygiene.
- LARGE VENUES (e.g., sit-down dining, movie theaters, sporting venues, places of worship) can operate under limited physical distancing protocols.
GYMS can remain open if they adhere to standard sanitation protocols. - BARS may operate with increased standing room occupancy, where applicable.
# # #